
Post by : Anees Nasser
Traditionally, disease monitoring was reactive; symptoms were often recognized only once outbreaks had spread or fatalities had occurred. In response, public health strategies were delayed, burdened by time-consuming data collection and ineffective communication.
However, as we enter 2026, this outdated model is rapidly evolving. With the integration of digital platforms, smart wearables, artificial intelligence, and interconnected systems, health authorities can now continuously monitor and swiftly react to emerging health threats. This transformation signifies a groundbreaking shift in our approach to understanding and managing diseases.
Traditionally, disease tracking relied on timely clinical reports, yet doctors and labs often faced delays. Such lags could span several weeks, allowing outbreaks to flourish before actionable trends were discerned.
By the time significant patterns emerged, containment efforts were frequently constrained, resulting in increased health risks and economic fallout.
Information was typically compartmentalized across various healthcare settings, making comprehensive data collection a challenge. This disunity hindered public health officials from grasping the full scale of emerging issues.
Modern techniques focus on the continuous accumulation of health data instead of relying on sporadic updates. Real-time information collection enables authorities to recognize evolving trends before they lead to significant outbreaks.
This capability allows for early interventions against minor indicators, like unusual symptom gatherings or increased absenteeism in the workplace.
In the realm of disease management, rapid detection equates to swift action—ultimately saving lives. Technology diminishes the delay between threat recognition and response, turning speed into a significant asset for public health.
Wearables like fitness trackers and smartwatches can monitor vital signs, sleep quality, and physical activity. Individually, these can aid personal health; meanwhile, when aggregated, they unveil vital population health trends.
Data harvested collectively can signal early indicators of disease spread, such as heightened heart rates or patterns of sleep disturbance across regions.
Unlike conventional methods that depend on patient self-reporting, wearables collect information passively. This feature minimizes the reliance on users actively sharing symptoms, capturing data from those who may not seek immediate care.
The integration of electronic health records is crucial for contemporary disease monitoring, facilitating real-time tracking of diagnoses and treatment results.
This harmonization offers a thorough view of disease severity and transmission patterns, enhancing situational awareness in times of public health crises.
Digital records help eradicate issues linked with manual reporting, employing standardized formats that simplify trend analysis across various regions.
The vast amounts of data generated by disease monitoring exceed human analytical capacity. AI excels at uncovering subtle patterns that would otherwise go unnoticed.
With the ability to identify unusual symptom patterns or geographical clusters early, AI serves as a vital early alert mechanism for health authorities.
Beyond mere detection, AI also forecasts potential disease trajectories based on factors such as mobility trends and climate variables, aiding governments in resource planning and preventive actions.
Human movement significantly impacts transmission rates. Anonymized mobile data provides insights into movement patterns, which affect regional disease spread.
Such data is crucial for tailored interventions, avoiding blanket measures.
The value of mobility data comes with privacy concerns; responsible monitoring mandates that data is anonymized, secured, and solely dedicated to public health.
Many diseases are affected by environmental variables like rainfall and humidity. Technological advancements allow health systems to incorporate environmental data into disease models.
By tracking conditions conducive to disease propagation, health authorities can preemptively act to mitigate outbreaks.
As climate change reshapes patterns of disease transmission, traditional monitoring systems face challenges. Technology enables more adaptive and effective surveillance methods.
Individuals often search health-related queries online before seeking medical attention. Analyzing these digital signals can help in identifying emerging health risks ahead of clinical data.
Integrating digital insights with traditional monitoring enhances early detection capabilities.
Not all online activity accurately reflects health trends. Advanced analytics are vital to differentiate genuine signals from seasonal noise.
Telemedicine platforms offer essential insights into symptoms and health patterns while reaching beyond physical healthcare facilities.
These remote consultations capture early-stage conditions that may otherwise go unnoticed, particularly in underserved areas.
By monitoring health remotely, telehealth systems help manage patient influx, reducing the need for unnecessary hospital visits during outbreaks.
Public health dashboards illuminate intricate datasets, enabling quick visualization of epidemic cases, healthcare capacity, and geographical data.
This transparency aids in faster, evidence-backed decision-making.
Well-managed dashboards foster transparency, enhancing public understanding during health crises and promoting cooperative responses to emergencies.
With advanced monitoring, public health responses can be more focused, enabling strategic interventions rather than sweeping policies.
This specificity minimizes both social disruption and economic impact while retaining effectiveness.
Tech-driven monitoring can identify susceptible populations sooner, allowing for targeted protective measures for those at heightened risk.
Collecting extensive health data raises ethical dilemmas. Protecting privacy, ensuring consent and preventing misuse are essential for sustaining public trust.
Robust governance is pivotal, as ineffective regulation can stymie public acceptance.
Not everyone has the same access to technology, which may inadvertently exclude marginalized populations from monitoring efforts without combining with traditional tactics.
A more inclusive approach is crucial to ensure fair health monitoring.
Data that favors certain demographic groups can result in overlooking others, leading to potential inaccuracies in responses.
Ongoing evaluation and adjustment are vital for equitable treatment.
Finding a balance between sensitivity and specificity is crucial; succumbing to false alarms can undermine trust and consume resources unproductively.
Human oversight remains a key component alongside automated detection systems.
Diseases disregard borders, highlighting the necessity for global data sharing. Technology enables cooperative surveillance, bolstering international preparedness and response.
Uniform data standards improve cross-country cooperation, accelerating overall health responses.
Technology's potential lies in prevention. Continuous monitoring empowers health systems to act preemptively, averting severe outbreaks.
This proactive stance diminishes suffering and economic loss, positioning disease monitoring as a strategic necessity.
As monitoring becomes a standard practice, disease surveillance evolves from episodic responses to integrated public health methodology.
Strong regulatory systems are crucial to guarantee ethical and effective usage of health technologies. Clear directives outline data access and accountability.
Effective governance determines whether technology fosters trust or detracts from it.
Clarifying how monitoring systems function and their significance enhances public support. Transparency alleviates fear and combats misinformation.
Future systems will advance beyond mere detection, striving to predict both individual and community health risks. Personalized alerts may soon become standard practice.
This shift signifies a proactive approach to healthcare protection.
Rather than replacing healthcare professionals, technology will enhance their capability to act swiftly and effectively.
The integration of technology in disease monitoring marks a pivotal transformation in public health. By converting dispersed data into actionable insights, societies can detect and manage health threats with unprecedented efficiency.
Though challenges related to privacy, equity, and accuracy persist, the trajectory is unmistakable. In 2026, the focus of disease monitoring is not merely on tallying cases, but on understanding health dynamics as they unfold. Used responsibly, technology not only tracks disease but also safeguards lives.
Disclaimer:
This article is intended for informational purposes only and should not be construed as medical or public health advice. Monitoring practices may differ globally.









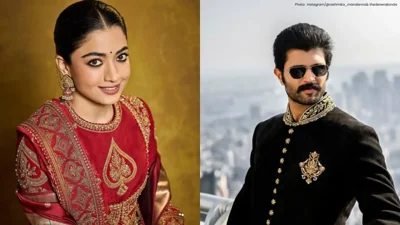
Rashmika Mandanna and Vijay Deverakonda to Tie the Knot on February 26
Rashmika Mandanna and Vijay Deverakonda are set to marry in an intimate Udaipur ceremony on February

FIFA Upholds 2026 World Cup Ticket Pricing Despite Fan Dissatisfaction
FIFA defends its ticket pricing for the 2026 World Cup, introducing a $60 tier to enhance affordabil

Trump Asserts Role in India-Pakistan Conflict Resolution, India Refutes Claims
Trump asserts he facilitated peace between India and Pakistan, but India firmly denies any US involv

Telangana Women Tragically Killed in California Car Accident, Families Request Assistance
Two Telangana women in the US die in a tragic car crash, prompting families to seek government suppo

Dhurandhar Achieves Remarkable Success, Surpassing ₹1100 Cr Worldwide
Ranveer Singh's Dhurandhar continues its box office dominance, crossing ₹1100 crore globally and sur

Asian Markets Climb as Dollar Weakens and Silver Surpasses $80 on Rate Cut Anticipation
Asian equities hit six-week highs while silver crosses $80, buoyed by expectations of Federal Reserv