Post by : Anees Nasser
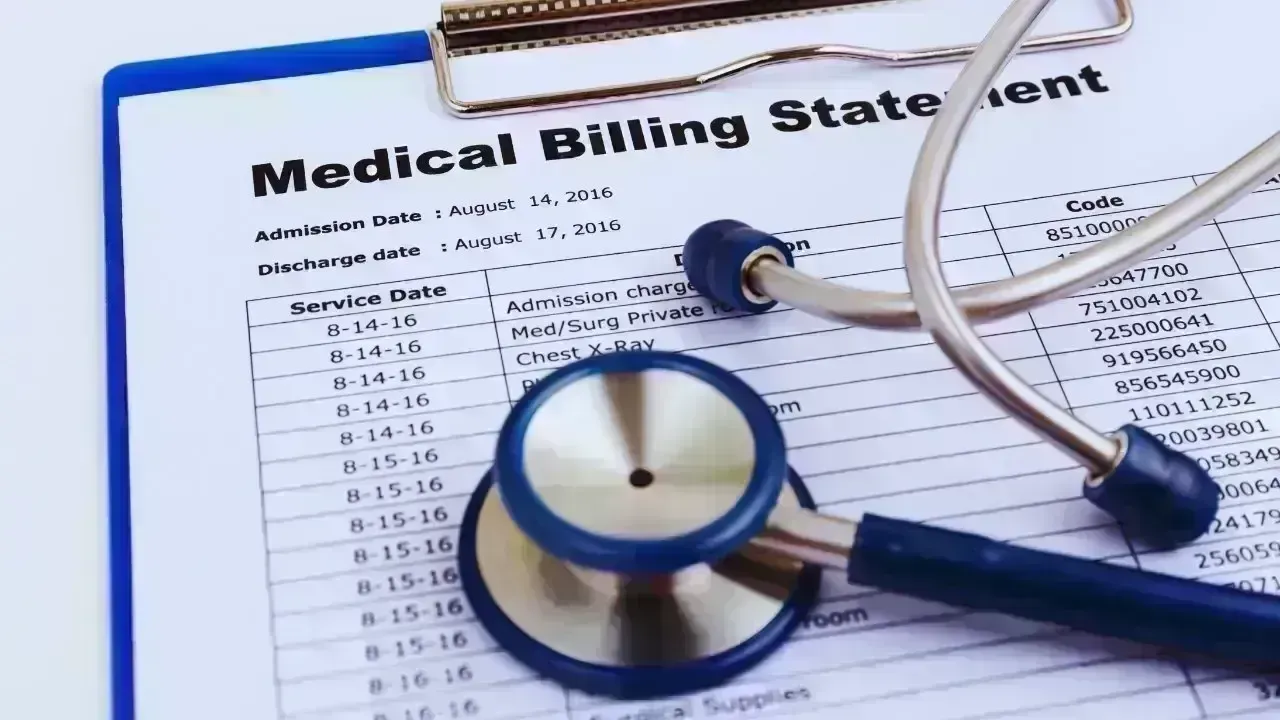
For most of modern history, healthcare was viewed as a social necessity—something societies collectively supported to ensure basic wellbeing. In recent years, however, healthcare has increasingly become a source of financial anxiety. In 2026, rising medical costs are no longer an abstract policy concern; they are a lived reality for millions of households.
From routine doctor visits and diagnostic tests to life-saving treatments and long-term care, healthcare expenses have climbed faster than incomes in many parts of the world. Even insured families find themselves paying more out of pocket, while governments struggle to balance public health obligations with fiscal limits. The result is a system where access to care is increasingly shaped by affordability, not just medical need.
One of the most persistent drivers of rising healthcare costs is medical inflation. Unlike general inflation, which affects everyday goods, medical inflation reflects the increasing cost of services, equipment, and treatments. In many countries, healthcare inflation consistently exceeds overall inflation rates.
This gap means that even when wages rise modestly, healthcare becomes less affordable. Households feel the pressure through higher insurance premiums, increased co-payments, and rising prices for medicines and procedures.
Medical innovation has saved countless lives, but it has also increased costs. Advanced diagnostics, specialised surgeries, personalised medicine, and cutting-edge therapies require expensive technology and highly trained professionals.
While these advancements improve outcomes, they also push healthcare spending upward. The dilemma is clear: better care often means higher costs, forcing difficult choices for individuals and policymakers alike.
Even with insurance coverage, families are paying more directly for healthcare. Deductibles, co-payments, uncovered services, and medication costs add up quickly. Routine care that once felt affordable now requires careful budgeting.
For middle-income households, this creates a precarious situation. They may earn too much to qualify for assistance but not enough to comfortably absorb medical expenses, leaving them vulnerable to financial shocks.
Medical expenses have become a leading cause of household debt in many regions. Unexpected illness or injury can wipe out savings, force families to borrow, or delay other essential spending such as education or housing.
This financial strain extends beyond the patient, affecting entire families and sometimes spanning generations.
Insurance is meant to provide security, but rising healthcare costs have pushed insurers to raise premiums and limit coverage. Many plans now cover fewer services or require higher contributions from policyholders.
As a result, insurance increasingly feels like a partial shield rather than full protection. People may hesitate to seek care, fearing costs even when insured.
Healthcare insurance systems have grown more complex, making it difficult for individuals to understand what is covered. Confusion leads to unexpected bills and delayed treatment, further eroding trust in the system.
Public healthcare systems are not immune to rising costs. Governments must fund hospitals, staff salaries, medicines, and infrastructure while managing limited budgets.
As healthcare spending consumes a larger share of public finances, difficult trade-offs emerge. Governments may reduce coverage, delay investments, or shift costs to patients through user fees.
Ageing populations significantly increase healthcare demand. Older adults require more frequent and complex care, including chronic disease management and long-term support.
This demographic shift places sustained pressure on public systems, driving costs higher year after year.
Drug development is costly, involving years of research, testing, and regulatory approval. Pharmaceutical companies argue that high prices are necessary to fund innovation.
However, pricing practices, patent protections, and limited competition often result in medicines that are unaffordable for many patients. Even essential drugs can carry price tags far beyond production costs.
High medication costs force patients to ration doses, delay refills, or abandon treatment altogether. This not only worsens health outcomes but can lead to higher costs later when untreated conditions become emergencies.
Digital health records, telemedicine platforms, and data systems promise efficiency, but they also require significant investment. Maintenance, cybersecurity, and system upgrades add to overall healthcare spending.
While technology improves care coordination, its financial benefits often take time to materialise, leaving short-term costs high.
Healthcare systems are burdened by administrative layers involving billing, insurance processing, compliance, and reporting. These non-clinical costs consume substantial resources that do not directly improve patient care.
Patients ultimately pay for this complexity through higher prices.
Rising healthcare costs deepen inequality. Wealthier individuals can afford private care, faster treatment, and advanced options, while lower-income groups face longer waits or reduced access.
This divide undermines the principle of healthcare as a universal right, turning it into a market-driven service.
Rural and marginalised populations often face higher indirect costs, including travel, time off work, and limited service availability. These factors compound financial barriers and discourage timely care.
Financial anxiety linked to healthcare costs affects mental wellbeing. Worrying about bills, insurance coverage, and future expenses adds emotional strain to already vulnerable moments.
This stress can worsen recovery and contribute to long-term mental health challenges.
Fear of costs leads many people to delay or avoid seeking care. What begins as a manageable condition can escalate into a serious illness, increasing both human and financial costs.
Preventive care—such as screenings, vaccinations, and lifestyle interventions—can reduce long-term healthcare costs. Yet preventive services are often undervalued or underutilised.
When prevention is neglected, healthcare systems pay more later through emergency treatments and chronic disease management.
Both individuals and policymakers sometimes prioritise short-term savings over long-term health investment. This approach reduces immediate spending but increases future costs, perpetuating the cycle of rising expenses.
Patients pay directly through bills, premiums, and lost income. Families absorb emotional and financial stress, often making sacrifices to support care.
The cost of healthcare reshapes household priorities, affecting education, housing, and retirement planning.
Public healthcare costs are ultimately borne by taxpayers. As spending rises, governments may increase taxes, reduce other services, or accumulate debt.
Healthcare affordability becomes a broader economic issue, influencing national budgets and policy debates.
Rising healthcare costs affect productivity. Ill health, delayed treatment, and financial stress reduce workforce participation and efficiency.
Businesses face higher insurance costs, while economies lose growth potential when healthcare becomes unaffordable.
Telemedicine can lower costs by reducing hospital visits and improving access. It offers convenience and efficiency, particularly for routine consultations.
However, technology alone cannot offset structural cost drivers such as pricing, administration, and demographic change.
Better data can improve care coordination and reduce duplication. While promising, these gains require upfront investment and systemic reform.
Some governments use regulation to control prices of medicines and procedures. While controversial, these measures can improve affordability if carefully designed.
The challenge lies in balancing cost control with innovation and quality.
Expanding healthcare access often increases spending initially. Long-term savings depend on effective management, prevention, and efficiency.
Policy choices today will determine whether healthcare remains accessible or becomes increasingly exclusive.
Viewing healthcare as an investment rather than a cost changes priorities. Healthier populations contribute more productively to society, reducing long-term expenditure.
This perspective supports greater emphasis on prevention and early intervention.
Public demand for affordable healthcare influences political action. Sustained pressure is often necessary to drive meaningful reform.
Structural factors—ageing populations, medical innovation, and chronic disease—suggest that healthcare costs will continue to rise.
The focus must shift from reducing costs outright to managing them fairly and sustainably.
A healthcare system’s success is increasingly judged by affordability and access, not just medical outcomes. Equity and sustainability are becoming central benchmarks.
The rising cost of healthcare is not just a financial issue—it is a social one. When people delay care, sacrifice essentials, or live in fear of medical bills, the consequences ripple through families, communities, and economies.
In 2026, the question is no longer whether healthcare costs are rising, but who absorbs the impact. Patients, families, governments, and societies all pay the price in different ways. Addressing this challenge requires more than incremental change. It demands a collective rethinking of how healthcare is funded, delivered, and valued.
Ultimately, the true cost of healthcare is measured not only in currency, but in wellbeing, equity, and trust. How societies respond to this challenge will define the future of health for generations to come.
Disclaimer:
This article is intended for informational and analytical purposes only. It does not constitute medical, financial, or policy advice. Healthcare systems and costs vary by region and over time.









Rashmika Mandanna and Vijay Deverakonda to Tie the Knot on February 26
Rashmika Mandanna and Vijay Deverakonda are set to marry in an intimate Udaipur ceremony on February

FIFA Upholds 2026 World Cup Ticket Pricing Despite Fan Dissatisfaction
FIFA defends its ticket pricing for the 2026 World Cup, introducing a $60 tier to enhance affordabil

Trump Asserts Role in India-Pakistan Conflict Resolution, India Refutes Claims
Trump asserts he facilitated peace between India and Pakistan, but India firmly denies any US involv

Telangana Women Tragically Killed in California Car Accident, Families Request Assistance
Two Telangana women in the US die in a tragic car crash, prompting families to seek government suppo

Dhurandhar Achieves Remarkable Success, Surpassing ₹1100 Cr Worldwide
Ranveer Singh's Dhurandhar continues its box office dominance, crossing ₹1100 crore globally and sur

Asian Markets Climb as Dollar Weakens and Silver Surpasses $80 on Rate Cut Anticipation
Asian equities hit six-week highs while silver crosses $80, buoyed by expectations of Federal Reserv